Background: Bispecific T-cell engagers antibodies (BiTEs) have shown promising efficacy across B-cell non-Hodgkin lymphoma (BCL) subtypes. If a response is observed, consolidation with allogeneic hematopoietic cell transplantation (alloHCT) could be reasonably pursued for high risk patients. To date, no data are available regarding BiTEs exposure prior to an alloHCT. Our aim was to describe patient characteristics, response, survival outcomes and treatment-related toxicities of patients treated with anti CD20-CD3 BiTE before alloHCT.
Methods: We performed a multicentric, retrospective study including adult patients (>18 years old) who received an alloHCT as consolidative therapy following anti-CD20-CD3 BiTE treatment for relapsed/refractory (R/R) BCL between February 2018 and March 2023. The primary endpoint was non-relapse mortality (NRM). Secondary endpoints were overall survival (OS), progression-free survival (PFS), relapse/progression of disease (Rl/POD), cumulative incidence of acute graft-versus-host disease (aGVHD) and chronic GVHD (cGVHD), and hematological recovery. Probabilities of OS and PFS were calculated using Kaplan-Meier estimator method, and NRM, RI/POD, GVHD and hematological recovery as cumulative incidences.
Results: A total number of 29 patients were included in the analysis. Patient's characteristics are described in Table 1. Median age was 57 (range 22-67) and 62.1% of patients were males. Twenty-four (82.8%) patients had stage III-IV at diagnosis and 21 (72.4%) were primary refractory. Nine (31%) patients had received an autologous transplant and 10 (34.5%), anti-CD19 CART prior to BiTE. Median number of lines at alloHCT were 4 (range 3-11). Median time from diagnosis to alloHCT was 39 (range 9 -208) months. Epcoritamab (n=16) was administered in monotherapy. Glofitamab (n= 13) was given in either monotherapy (n=2) or combination with either atezolizumab (n=2), polatuzumab (n=3) or englumafusp (n=6). The median number of BiTE's administered doses was 10 (range 4-20). The median time between BiTE's last dose and alloHCT was 44 (range 13 - 203) days.
Median follow-up among survivors was 21.9 months (range 3.3 - 52.6 months). At 18-months, OS, PFS, NRM and RI/POD were 66% (95% confidence interval [CI]: 45-81%), 62% (95% CI: 40-78%), 33% (95% CI: 15-53%), and 4% (95% CI: 0-12%), respectively. Causes of death were 1 relapse and 9 transplant toxicities (7=infections, 1=cGVHD, 1=cerebrovascular disease). Fifty-five percent of toxicity-related deaths were observed during the first 3 months from transplant. The cumulative incidence of neutrophil and platelet engraftment at day +30 was 90% (95% CI, 78-100%) and 68% (95% CI, 50-86%), respectively. The cumulative incidence of all grade and grade II-IV aGVHD at day +100 was 31% (95% CI: 13-49%) and 22% (95% CI: 7-37%), respectively. The cumulative incidence of all grade cGVHD at 18 months was 16% (95% CI: 2-30%), with only 1 patient presenting with moderate cGVHD. On univariate analysis, no prognostic factors were found in terms of OS, PFS, RI/POD and NRM.
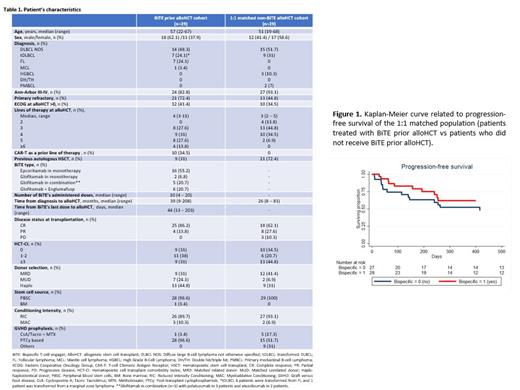
A comparison with a contemporary cohort of alloHCT recipients for BCL (N=101) from the Grupo Español de Trasplante y Terapia Celular (GETH-TC) who were not exposed to BiTE was performed ( figure 1). Propensity score matching using most significant patient, disease and alloHCT characteristics was performed to reduce cohort's heterogeneity ( Table 1). In the final 1:1 matched population (n=58; 29 patients treated with BiTE prior alloHCT and 29 patients who did not receive BiTE prior alloHCT), no differences in terms of OS, PFS, RI/POD and NRM at 18 months were observed (66% [95% CI, 45-81%] vs 48% [95% CI, 29-65%] [p=0.18]; 62% [95% CI, 40-78%] vs 45% [95% CI, 27-62%] [p=0.17]; 33% [95% CI, 14-52%] vs 41% [95% CI, 22-60%] [p=0.35] and 4% [95% CI, 0-10%] vs 10% [95% CI, 0-20%] [p=0.24].
Conclusions: We describe for the first time the results of BiTE exposure before alloHCT in terms of safety and efficacy. AlloHCT as consolidation therapy is feasible and does not seem to be detrimental for transplant outcomes in patients with R/R BCL with expected toxicity and surprisingly low relapse rate.
Disclosures
Kwon:Pfizer: Speakers Bureau; Jazz: Speakers Bureau; Kite-Gilead: Consultancy, Speakers Bureau. Lopez Corral:Novartis: Honoraria, Other: travel support; Gilead Sciences: Honoraria, Other: travel support; Janssen: Honoraria, Other: travel support. Mussetti:Gilead: Research Funding; Takeda: Honoraria; BMS, Jazz Pharaceuticals: Consultancy. Sureda Balari:MSD: Research Funding; Kite: Consultancy, Speakers Bureau; Takeda: Consultancy, Honoraria, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal